On this page, you will find:
- The final report
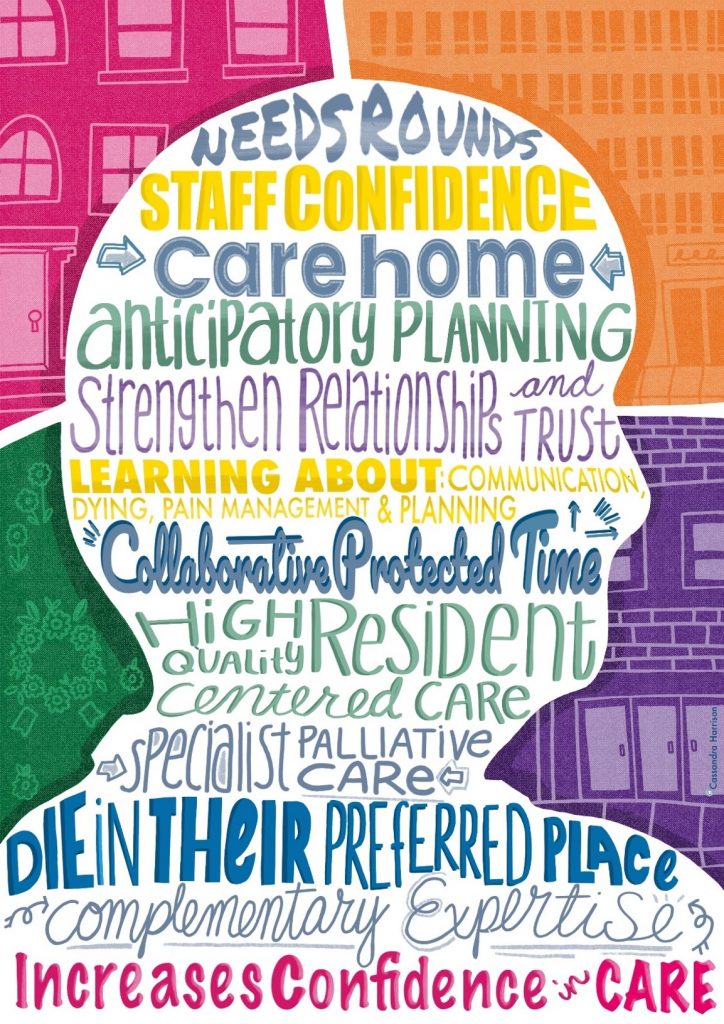
- An image that summarise how Needs Rounds work and their outcomes in the UK
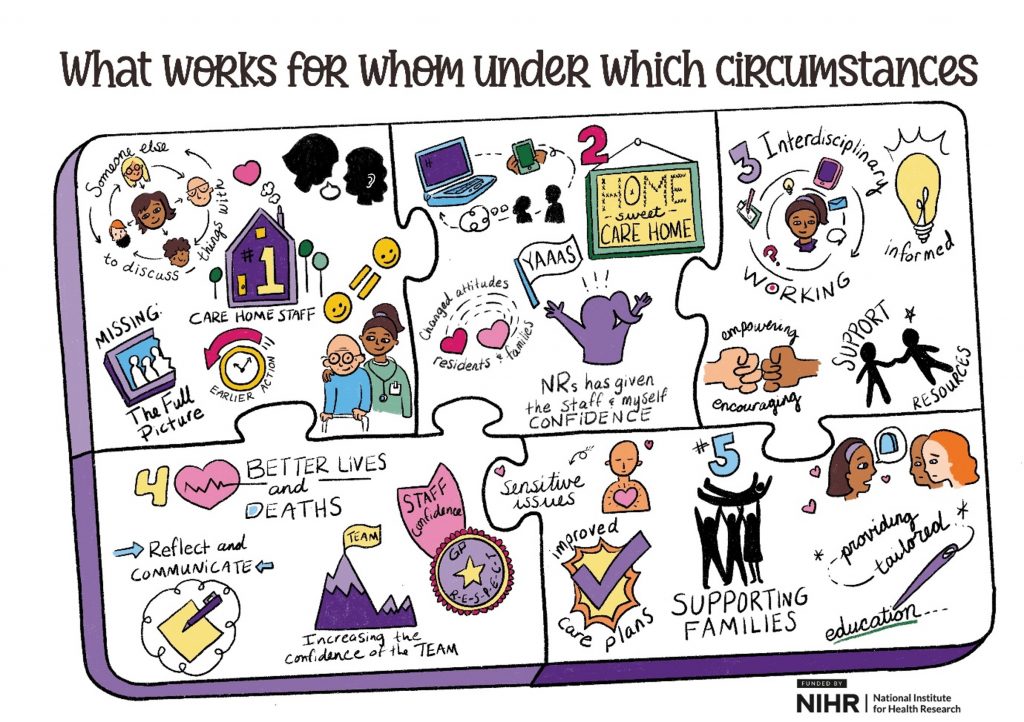
- An image that summarise what Needs Rounds offer
- A poster presented at the 2023 Oceanic Palliative Care Conference
- A list of academic papers and findings for you to read.
The final report
The funder published the final report in July 2024. You can access it for free here.
This report should be referenced as follows:
Forbat L, Macgregor A, Spilsbury K, McCormack B, Rutherford A, Hanratty B, et al. Using
Palliative Care Needs Rounds in the UK for care home staff and residents: an implementation
science study. Health Soc Care Deliv Res 2024;12(19). https://doi.org/10.3310/KRWQ5829
How and why do Needs Rounds work?
The following image summarises the main theory from the UK work.
Needs Rounds can provide care home staff and specialist palliative care staff with the opportunity to collaborate during a protected time, to plan for residents’ last months and weeks of life. Needs Rounds augment existing practice by building care home staff confidence for those who attend, and prompting anticipatory planning and care. Needs Rounds can strengthen relationships and trust, and shift power dynamics between care home and hospice services by harnessing complementary expertise. Integrating learning into Needs Rounds strengthens understandings of the dying process, symptom and pain management, advance/anticipatory care planning, and communication mechanisms between care home staff, families, specialist palliative care staff and primary care. This leads to high quality resident centred care, enabling residents to be cared for and die in their preferred place. Needs Rounds also benefit relatives by increasing their confidence in care quality and care home staff, by providing timely expert input.
Pulling together different parts of the puzzle
In the first year of the UK study we developed 5 ideas about what would work, for whom, under what circumstances and why, when using Needs Rounds. The data we gathered through interviews and discussions are summarised in the jigsaw diagram.
- If care homes and specialist palliative care don’t work together, then there’s part of the picture/expertise missing.
- Needs Rounds can help staff feel more confident in the care they give.
- Working across disciplines is encouraging and useful for everyone. Working across disciplines includes care homes and specialist palliative care, but also GP practices, hospitals, pharmacy and the ambulance service.
- The aim is to have better lives and deaths of residents in care homes, this is achieved through improved communication
- Needs Rounds help support families. The tailored education helps care home staff talk with families about current and future care needs, including the most sensitive of topics for when the resident is in the last weeks and days of life.
Patient and Public Involvement and Engagement
Here you can see a poster presented at the Oceanic Palliative Care Conference, September 2023, on the patient and public involvement and engagement work. You can download the file to read the whole document.
Academic papers
The links take you straight to the abstract/summary of the paper. If you’d like to learn more and can’t access the whole paper, please email the team.
- Forbat, L et al. (2024) Negotiating pace, focus and identities: Patient/public involvement/engagement in a palliative care study Sociology of Health and Illness doi.org/10.1111/1467-9566.13785.
- Macgregor A, et al. (2023) Supporting care home residents in the last year of life through ‘Needs Rounds’: Development of a pre-implementation programme theory through a rapid collaborative online approach. Frontiers in Health Service Research – Implementation Science. 2:1019602. doi: 10.3389/frhs.2022.1019602.
- Koerner, J,. et al. (2021) Context and mechanisms that enable implementation of specialist palliative care Needs Rounds in care homes: Results from a qualitative interview study. BMC Palliat Care 20, 118 (2021).
- Macgregor, A,. et al (2021) Palliative and end of life care in care homes: Protocol for co-designing and implementing an appropriate scalable model of Needs Rounds in the United Kingdom. BMJ Open 2021;11:e049486.
- Forbat, L,. et al (2020) Reducing time in acute hospitals: a stepped wedge randomised control trial of a specialist palliative care intervention in residential care homes. Palliative Medicine. 34(5):571-579.
- Liu, W-M, et al. (2020) Improved quality of death and dying in care homes: a palliative care stepped wedge randomised control trial in Australia. Journal of the American Geriatrics Society. 68(2): 305-312.
- Johnston, N,. et al (2019) Normalising and planning for death in residential care: Findings from a qualitative focus group study of a specialist palliative care intervention. BMJ Supportive and Palliative Care. 9(1) e12.
- Forbat, L,. et al (2018) Improving specialist palliative care in residential care for older people: a checklist to guide practice. BMJ Supportive and Palliative Care. 8(3): 347-353.
- Chapman, M,. et al. (2018) Avoiding costly hospitalisation at end of life: Findings from a specialist palliative care pilot in residential care for older adults. BMJ Supportive and Palliative Care. 8(1):102-109